HIV and smoking are a costly and deadly combination that absorbs significant Medicaid dollars.
In 2022, the federal government spent an estimated $13 billion on Medicaid services for people with HIV. Additionally, state Medicaid spending totaled an estimated $5.4 billion in the same year.
Antiretroviral therapies have provided the ability to live longer for those with HIV. In fact, some groups with HIV have a similar life expectancy to the general population.
But while antiretroviral therapies are allowing people to have more time, cigarettes are taking it away.
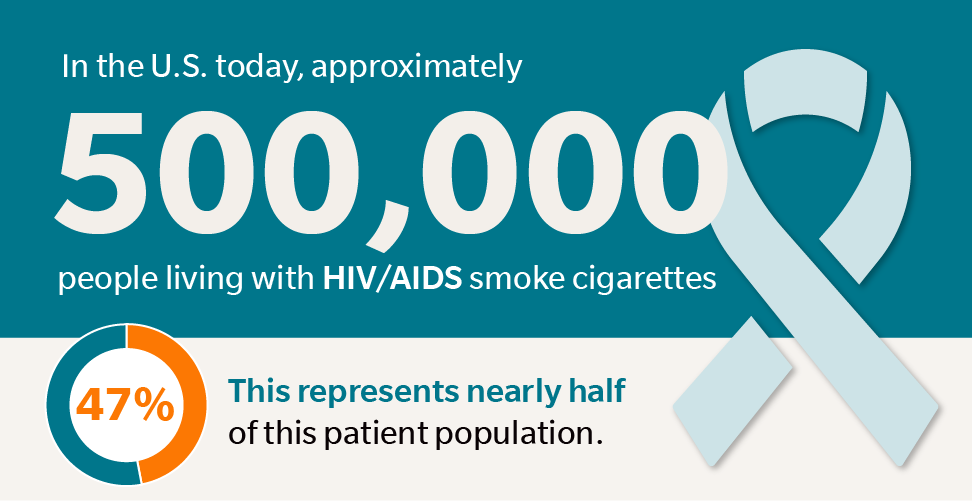
In the U.S. today, approximately 500,000 people living with HIV/AIDS smoke cigarettes. This represents nearly half (47%) of this patient population.
Cigarette smoking is one of the leading causes of death in this group and is a main driver of the differences in survival rates between people with HIV and people without HIV.
3 Key Things to Know about HIV and Smoking
People who smoke and have HIV are more likely to get serious illnesses than nonsmokers with HIV, including lung cancer and cardiovascular disease.
- Increased risk of lung cancer, at younger ages. Those who smoke and have HIV are more likely to get lung cancer than nonsmokers with HIV and to acquire it at younger ages. In fact, lung cancer is the leading cause of cancer death among people with HIV on antiretroviral therapy. It is estimated that 94% of lung cancer diagnoses among those with HIV could potentially be prevented by eliminating cigarette smoking in this population.
- Higher rates of hypertension. High blood pressure is more common among people with HIV, with a prevalence of >42% vs. 29% in the general population. People with HIV have poorer blood pressure control and higher rates of hypertension-associated morbidity. Improving blood pressure among HIV positive people who smoke could have tremendous life-saving impacts.
- Higher rates of hyperlipidemia. High cholesterol, also known as hyperlipidemia, is extremely common among people with HIV, with rates exceeding 60% in some population-based studies. It is an important contributor to the excess risk of cardiovascular events and mortality in this population.
Blood pressure and lipid abnormalities are amplified by smoking, making their control that much more important among tobacco users.
A Paradigm Shift to Improve the Health of People with HIV
To date, the relatively few smoking cessation trials conducted among people with HIV have yielded quit rates of only 13-15%. What this means is that over 85% of HIV patients who are smoking today will continue to smoke for the foreseeable future.
A paradigm shift is needed that focuses on improving the outlook of all HIV positive smokers, including those who continue to use cigarettes.
We are participating in a randomized trial funded by the National Cancer Institute that will test a harm-reduction approach aimed at reducing the risks of cancer and cardiovascular disease in smokers with HIV.
Led by HIV physician and tobacco treatment expert, Dr. Jonathan Shuter at the Albert Einstein College of Medicine, the study brings together leading experts in internal medicine, harm reduction, behavioral science, infectious disease, cardiovascular risk reduction, and digital health.
Beginning in early 2024, the study will recruit 400 HIV-positive patients who smoke. All participants will be offered a 12-week course of prescription medication for quitting (varenicline/Chantix) plus evidence-based treatment for smoking cessation tailored to HIV positive smokers through the EX Program.
Half of participants will also receive clinic-based assistance to reduce cigarettes per day (in those who do not quit), undergo lung cancer screening, and meet with a cardiology care team to address blood pressure and lipid management.
The primary outcomes of the trial are 5 key harm-reduction metrics:
- Change in cigarettes smoked per day,
- The percentage that complete lung cancer screening,
- Improvements in systolic blood pressure,
- Improvements in total cholesterol, and
- Improvements in an overall score of cardiovascular disease risk.
The study will also provide important data about the cost effectiveness and feasibility of sustaining this treatment approach in medical centers across the U.S.
This exciting new research will introduce a novel harm reduction strategy for HIV-positive smokers that utilizes resources already in use in many, if not most, HIV care centers in the U.S.
See more insights on research underway or completed by EX Program experts in our Research section. To learn more about the outcomes of the EX Program for participants and health plans, please complete a Contact Us form today.