24.9% vs. 10.7%.
That’s the difference in smoking rates between adults on Medicaid and those with private health insurance. Given the deadly effects of smoking from head to toe, this staggering disparity cannot be ignored.
Coverage of cessation treatments to help Medicaid enrollees quit smoking has improved in recent years. But a recent study in Nicotine & Tobacco Research shows, on average, fewer than 10% of Medicaid enrollees with a past-year quit attempt received cessation medication and fewer than 3% received cessation counseling.
Together, we can do better.
Where more focus is needed to make an impact with help to quit smoking
The Nicotine & Tobacco Research study revealed how increased coverage of cessation treatment hasn’t necessarily translated into increased use of these treatments:
- Among the 37 states reporting quit medication claims, on average, 9.4% of fee-for-service Medicaid smokers who made a past-year quit attempt had claims for cessation medications. This rate varied widely from 0.2% in Arkansas to 32.9% in Minnesota.
- Among 20 states that maintain data on FFS Medicaid smokers who receive counseling, on average, 2.6% of these smokers who made a past-year quit attempt received counseling, ranging from 0.1% in Florida to 5.6% in Missouri.
The number of Medicaid FFS enrollees who received cessation treatment varied substantially across states, due to numerous reasons. Differences in state Medicaid cessation coverage and coverage barriers (such as the need for prior authorization to get quit medication) and differences in efforts to promote cessation among Medicaid enrollees certainly play a role.
Health plans that table finding ways to better help Medicaid enrollees quit smoking do so at their own peril. Medicaid spending for cessation medications and counseling is estimated at just over $13 million, compared to $45.9 billion that Medicaid spends annually on treating smoking-related diseases.
And these numbers could grow higher. An estimated 21% of Americans are covered by Medicaid—but that number is pre-pandemic. Medicaid enrollment has increased by more than 5 million from February to August 2020.
How digital can increase utilization of cessation treatments
After evaluating differences between the states, researchers concluded that “insurance coverage for smoking cessation treatment that is comprehensive, barrier-free, and widely promoted increases utilization of cessation treatments, leads to higher rates of successful quitting, and is cost-effective.”
One way to make cessation medication and counseling easier to access is through a digital health solution. In a comprehensive synthesis of the evidence, the Surgeon General recommends digital solutions as an effective way to support tobacco cessation, especially since they can help overcome accessibility issues for those who are low income and/or might lack transportation for going to a pharmacy or in-person coach.
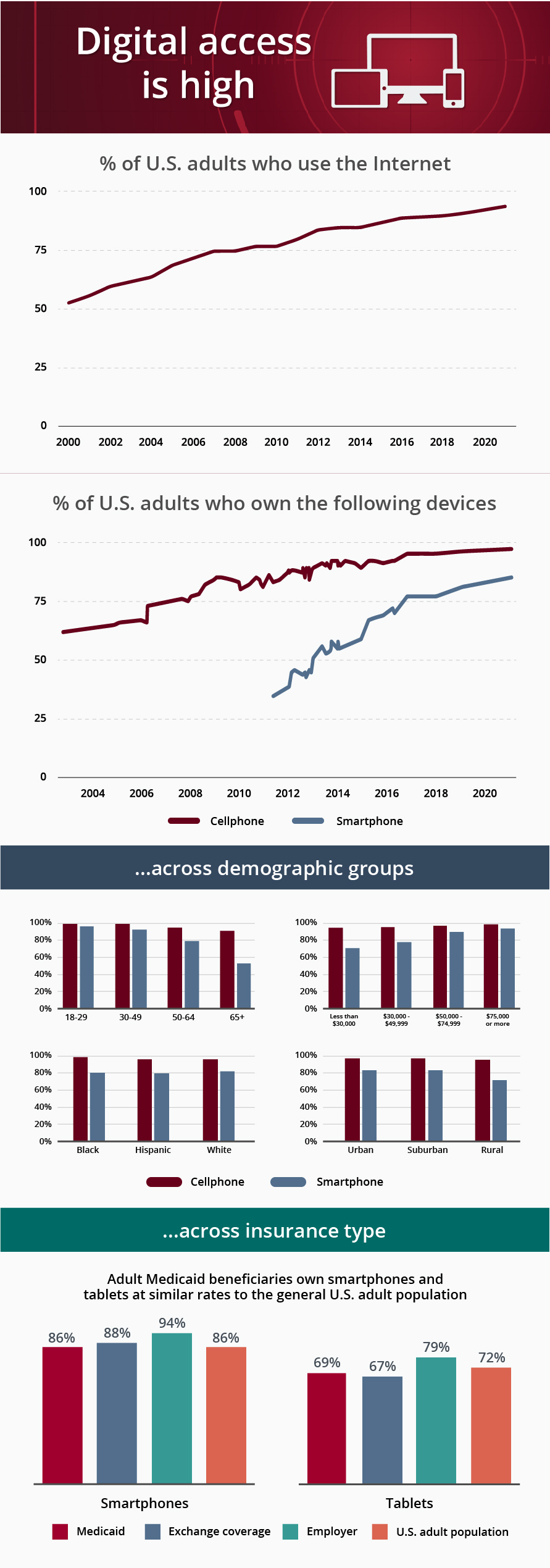
Wondering about the digital divide? Keep in mind that many Medicaid enrollees now own smartphones and tablets at similar rates to the general U.S. adult population. This means giving them access to digital programs can help cessation programs reach those who need them most.
Sources: www.pewresearch.org/internet/fact-sheet/internet-broadband/ www.pewresearch.org/internet/fact-sheet/mobile/ www2.deloitte.com/us/en/insights/industry/public-sector/mobile-health-care-app-features-for-patients.html
The EX Program, for example, offers live chat coaching with tobacco treatment specialists—in English or Spanish—from anywhere for help to quit smoking. Coaches can easily match participants up with nicotine patches, gum, or lozenges that are then shipped directly to the participant’s home.
See our blog, Is Live Chat Coaching an Effective Quit Smoking Method?, for more details about the value of live chat coaching for tobacco addiction.
Improved access alone is not the answer
While solving access is critical, it’s still only part of the equation. Making sure Medicaid enrollees understand that the support is available is just as equally critical. To do this, it requires a strong partnership between a health plan and tobacco cessation provider to innovate how promotions are done.
As the study noted, cessation counseling and medications work well for Medicaid enrollees—if they’re given those options. The researchers conclude, “Covering these treatments with minimal barriers and promoting this coverage so that Medicaid smokers and their providers are aware of and use the covered treatments are essential.”
When health plans commit to engaging Medicaid enrollees in quit-tobacco programs, it’s a win-win for everyone. Enrollees reap the benefits of better physical, emotional, and financial health that living tobacco-free affords, while health plans can impact health outcomes and generate meaningful savings on treating smoking-related diseases.
Let’s start a conversation to see how we can engage more of your Medicaid populations in help to quit smoking. Contact us to see a demo today.