When it comes to healthcare costs, you likely know that smoking is behind expensive heart and lung disease, as well as numerous cancers.
But individuals who smoke also have major problems when it comes to bones, joints, tissues, ligaments, and tendons.
The result?
More sick time for them and more healthcare spending for you.
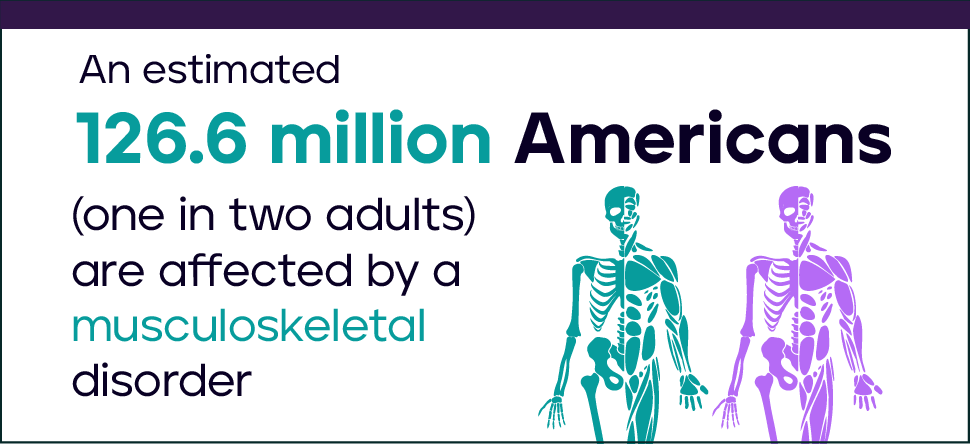
An estimated 126.6 million Americans (one in two adults) are affected by a musculoskeletal disorders (MSD)—comparable to the total percentage of Americans living with a chronic lung or heart condition—costing an estimated $213 billion in annual treatment, care, and lost wages.
But what does that mean on an individual employee basis?
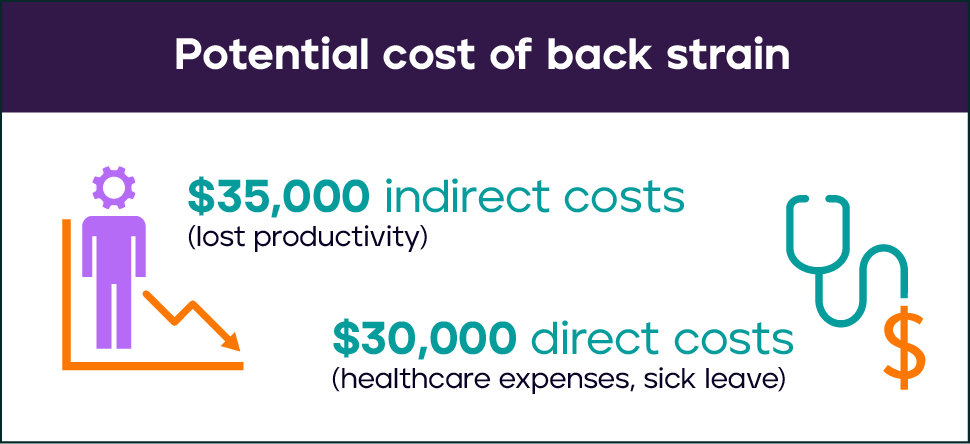
The OSHA’s Safety Pays cost calculator can total up the direct and indirect costs of a common MSD injury. Let’s take back strain as an example, which might have around $30,000 in direct costs related to healthcare expenses and sick leave. That same issue could result in about $35,000 in indirect costs, like lost productivity. And that’s just from one event. What if this employee has a couple back pain events every year?
For many companies, addressing this staggering cost is a high priority. In the Business Group on Health’s 2024 Large Employer Health Care Strategy Survey: Executive Summary, 75% of employers ranked musculoskeletal conditions among the top 2 health conditions driving their costs.
Yet, there’s another big strategy to consider when trying to manage MSD costs: Tobacco cessation.
What are musculoskeletal disorders?
MSD includes a wide range of diagnoses, including:
- Carpal Tunnel Syndrome
- Tendonitis
- Muscle/tendon strain
- Ligament sprain
- Tension Neck Syndrome
- Rotator Cuff Tendonitis
- Radial Tunnel Syndrome
- Trigger finger/thumb
- Mechanical Back Syndrome
- Degenerative Disc Disease
- Ruptured/herniated disc
These are sometimes referred to as repetitive motion injury, repetitive stress injury, or overuse injury. However, calling them that oversimplifies the fact that many risk factors lead to MSD, including tobacco use.
4 ways tobacco makes musculoskeletal disorders much worse
Providing treatment for MSD without addressing tobacco use is treating the symptom instead of the cause. Here’s why:
- Smoking has been shown to have a weakening effect on bones, because it reduces the blood supply to the skeletal system as well as surrounding tissues. Also, nicotine slows production of osteoblasts—the cells responsible for bone formation—so lost bone density isn’t replaced. Smokers absorb less calcium from their food as well, which is another big hit for bone mineral development.
- Tobacco use weakens tissues around the joints, which can lead to chronic injury and disease such as bursitis and tendonitis. The American Academy of Orthopaedic Surgeons has found rotator cuff tears in smokers are nearly twice as large as those in nonsmokers, most likely because the tendons in smokers are weaker.
- Smoking is linked to higher risk of low back pain, in large part because of the degenerative effect on bones, ligaments, and tendons. Smoking reduces the flow of nutrients to joints and muscles, so if tobacco use isn’t addressed, an employee will continue to weaken that area. That’s a huge deal, considering that back pain is one of the top reasons that employees call in sick and take disability leave.
- Tobacco use slows wound healing, because of decreased blood supply to tissues. That means smokers have a higher rate of complications after surgery, as well as higher risk of infection. A wound that may have been healed quickly in a nonsmoker then becomes a potentially long-term problem in a smoker, driving up healthcare expenditures and lowering productivity.
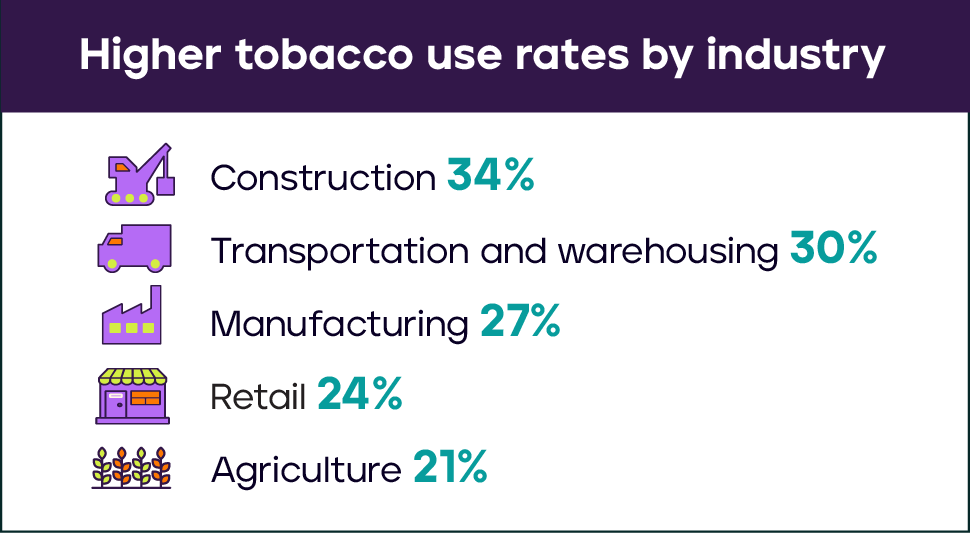
Certain industries have higher prevalence of MSD, including manufacturing, retail, transportation, agriculture, and construction. Perhaps not coincidentally, these are industries that also see high rates of tobacco use.
Because of these exacerbating effects, tobacco use makes MSD costs even higher. Doing something about tobacco use—and making it digital so employees can access it from anywhere—is key for improving engagement and reach for your quit-tobacco program.
Tailored, innovative approach to help employees quit
Tobacco users are more likely to quit successfully when they receive help that is tailored not only to the type of tobacco product they choose, but also specific to how they prefer to receive support and coaching.
For those with MSD, tobacco cessation can make a significant difference in terms of how the disorder progresses—or doesn’t. That can save you enormous healthcare costs in the future, and also strengthen your workforce into one that’s healthier, happier, and more productive.
To do that, employers need innovative programs that meet employees’ needs, including:
- Discrete live chat coaching with tobacco treatment specialists to tap into while on a job site
- An online community to connect 24/7 with peers who are facing the same challenges and who have successfully quit
- Dynamic text messaging to get support before or after a shift
- Free quit medication that’s delivered right to their home
- Tailored quit plan by quit status, program use, age, and tobacco use type (including menthol use)
- A digital, mobile-friendly library of evidence-based resources
EX Program delivers all of this and more. To start a conversation and see how we can engage more of your population in quitting tobacco, please contact us today.